Targeting the TME and Its Role in Cancer Development and Drug Resistance
The Tumor Microenvironment (TME) is the complex, heterogeneous cellular environment surrounding a tumor. The TME contains immune and inflammatory cells, blood vessels, fibroblasts and myofibroblasts, extracellular matrix (ECM), and a vast array of signaling molecules 1. The dynamic interactions between tumor cells and the TME largely determine whether the primary tumor metastasizes (develops secondary malignant growths elsewhere in the body), becomes dormant, or is eradicated. This makes the TME a prime target for both research and therapeutic intervention.
In this article, we will delve into the role of the TME in cancer development and drug resistance, the importance of research to better understand the TME, and TME-based biomarkers and therapeutic strategies.
Role of the Tumor Microenvironment in Cancer Development
The TME has a significant impact on the three main stages of cancer development (also known as tumorigenesis); tumor initiation, growth, and progression. Firstly, the TME facilitates angiogenesis (the process of new blood vessel formation): a key requirement in tumorigenesis. The TME does this by releasing pro-angiogenic factors, promoting the establishment of a vascular network that supplies the growing tumor mass with the necessary oxygen and nutrients, supporting tumor growth and metastasis 2.
A growing body of evidence highlights the contributions of innate and adaptive immune cells to tumor progression 3. By creating an immunosuppressive environment that inhibits the ability of immune cells to recognize and eliminate the malignant cell, the TME mediates immune evasion: another pivotal aspect of cancer progression 4. This is achieved by various mechanisms including the expression of immune checkpoint molecules and the recruitment of immunosuppressive cell populations.
Tissue remodeling, facilitated by components of the TME, is another significant contributor to tumor progression. This process involves alternating the ECM and the surrounding tissue architecture to accommodate the expanding tumor mass and facilitate invasion and metastasis 5.
The Tumor Microenvironment and Drug Resistance
The ability of the TME to influence tumor growth, progression, and metastasis is closely interlinked to its ability to induce drug resistance, impeding therapeutic efficacy and leading to persistent residual disease and recurrence 6. TME-mediated resistance can be broadly divided into two categories: inherent and acquired resistance 7. Inherent or intrinsic resistance is present without selective pressure from drug exposure and is based on the interactions of the TME with the cancer cells. Acquired resistance occurs in response to therapy and can result in pronounced changes to the TME.
Several studies have highlighted the TME’s ability to induce resistance to chemotherapy, targeted therapies, and immunotherapies by various mechanisms. Chemotherapy, a cornerstone of cancer treatment, targets rapidly dividing cells, but the TME can shield cancer cells from the full effects of chemotherapeutics 8. In the case of targeted therapies designed to interfere with specific molecules that aid cancer growth, the TME can activate alternative signaling pathways that enable the cancer cells to bypass the intended effects 9. Immunotherapy aims to stimulate the immune system to attack cancer cells, but the ability of the TME to suppress the immune response can render these treatments less effective 10.
The ability of the TME to impede drug delivery and enhance cancer cell survival is multifaceted. One mechanism involves the formation of a dense ECM that surrounds the tumor cells and acts as a physical barrier to drug penetration 11. This is directly linked to a reduced supply of oxygen, nutrients, and metabolites, which induces hypoxia and metabolic stress. Crucially, the resulting stress response pathways activate anti-apoptotic (apoptosis is a form of cell death) and drug resistance pathways 11.
Furthermore, the release of angiogenic factors promotes angiogenesis, and the resulting disorganized network of blood vessels can act as a physical barrier. This further impedes drug delivery while providing the cancer cells with the required nutrients for survival 2. Additionally, the TME can induce cellular dormancy, in which cancer cells become temporarily inactive, making them less susceptible to therapies that target dividing cells 12.
Therapeutic Targeting of the TME
The considerable impact of the TME on tumor initiation, progression, and metastasis has rendered it a promising therapeutic target for many years. More recently, as research has continued to shed light on the ability of the TME to induce drug resistance, there has been another surge of interest in developing therapies that target TME’s adaptive mechanisms as a way to enhance the effectiveness of traditional cancer treatments and minimize the probability of relapse.
Current strategies for TME modulation are diverse and have focused on modulating various components of this environment. For example, immune checkpoint inhibitors (ICIs), which have revolutionized cancer treatment in the last decade, work by blocking specific molecules in the TME that prevent the immune system from attacking cancer cells 13.
Another approach is angiogenesis inhibitors, which can starve the tumor of nutrients. However, several studies have shown that targeting angiogenesis as a therapeutic strategy using VEGF inhibitors accelerated metastasis and enhanced the tumor’s aggressiveness due to the TME’s activation of drug resistance pathways that release additional angiogenic factors 14,15.
Emerging approaches include the use of CAR-T cell therapy, a type of immunotherapy where patients’ T-cells are genetically modified to recognize and kill cancer cells 16, and the development of stromal modulating agents, which aim to reprogram the stromal cells in the TME that often promote tumor growth and therapeutic resistance 17.
TME Biomarkers and Personalized Medicine in Oncology
Recently, cancer research and therapeutics have begun to shift from a one-size-fits-all approach to a more individualized strategy known as personalized medicine in oncology 18. Due to our growing understanding of how the TME influences cancer progression and treatment outcomes, identifying cancer biomarkers within the TME is crucial for guiding therapeutic decisions and predicting treatment responses 19.
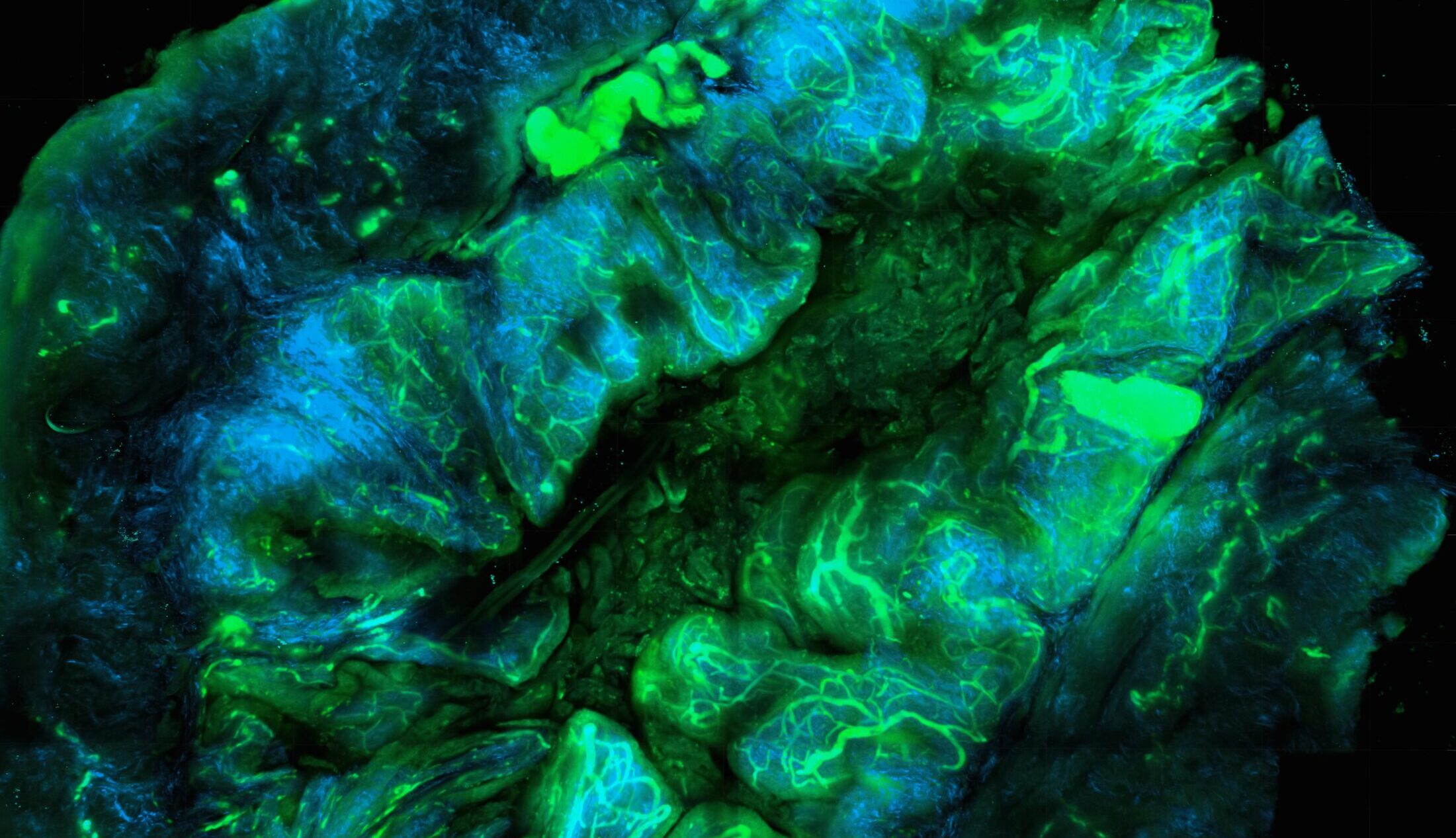
Comprehensive genetic profiling of the TME is required to identify potential biomarkers that may determine cancer progression or treatment responses 20,21. This is generally achieved through a combination of immunohistochemistry (IHC) and tumor gene expression profiling by high-throughput omics methods – genomics, proteomics, metabolomics, and transcriptomics – on patient samples, often provided by biobanks such as Audubon Biosciences.
Recent advances in these methodologies, such as novel high-resolution spatial transcriptomics technologies 22,23, have enhanced our knowledge of the TME and accelerated our ability to identify novel cancer biomarkers 24,25. Following identification, biomarkers must be validated in preclinical and clinical studies, to ensure the biomarker accurately predicts the expected outcome (i.e., treatment response or survival) 26.
TME biomarkers are extremely valuable for predicting therapeutic outcomes. For example, the presence of a specific population of immune cells within the TME can provide valuable insights into how a patient might respond to immunotherapy 27. Thus, TME biomarkers are powerful tools for guiding therapeutic decisions, resulting in improved outcomes and reduced healthcare costs.
Research Advances and Future Directions
Ongoing research efforts are striving to attain a better understanding of the complex interactions between the TME and cancer cells. A particular focus is on the role of immune cells, particularly T-cells, in the TME, as research has shown these have the potential to drastically impact treatment outcomes and cancer progression. Researchers are investigating the potential of ICIs to inhibit the TME’s evasion of immunotherapies 27 One aspect of this research is identifying and validating novel cancer biomarkers that could predict responses to ICIs.
In the future, cancer therapy is likely to shift dramatically towards a more personalized medicine model, meaning that reliable biomarkers and a thorough understanding of distinct, cancer-conferring molecular mechanisms will be pivotal for developing safe and effective personalized therapeutic strategies 19. Human biosamples play an essential role in the development of TME-targeting therapies, as they are required to better our understanding of TME-tumor interactions and to identify the specific biomarkers necessary for personalized therapeutic targeting of the TME.
Conclusion
A deep understanding of the complex, intricate interactions between the TME and cancer cells is vital for developing novel cancer biomarkers and more effective therapies. To learn more about how human biosamples can accelerate TME research, visit our dedicated product page to browse our products and request a quote, or get in touch today.
References:
- Anderson NM, Simon MC. The tumor microenvironment. Curr Biol. 2020;30(16):R921-R925. doi:10.1016/j.cub.2020.06.081
- Kim HJ, Ji YR, Lee YM. Crosstalk between angiogenesis and immune regulation in the tumor microenvironment. Arch Pharm Res. 2022;45(6):401-416. doi:10.1007/s12272-022-01389-z
- Hinshaw DC, Shevde LA. The Tumor Microenvironment Innately Modulates Cancer Progression. Cancer Res. 2019;79(18):4557-4566. doi:10.1158/0008-5472.CAN-18-3962
- Becker JC, Andersen MH, Schrama D, Thor Straten P. Immune-suppressive properties of the tumor microenvironment. Cancer Immunol Immunother. 2013;62(7):1137-1148. doi:10.1007/s00262-013-1434-6
- Winkler J, Abisoye-Ogunniyan A, Metcalf KJ, Werb Z. Concepts of extracellular matrix remodeling in tumour progression and metastasis. Nat Commun. 2020;11(1):5120. doi:10.1038/s41467-020-18794-x
- Meads MB, Gatenby RA, Dalton WS. Environment-mediated drug resistance: a major contributor to minimal residual disease. Nat Rev Cancer. 2009;9(9):665-674. doi:10.1038/nrc2714
- Klemm F, Joyce JA. Microenvironmental regulation of therapeutic response in cancer. Trends Cell Biol. 2015;25(4):198-213. doi:10.1016/j.tcb.2014.11.006
- Wang S, Li Y, Xing C, et al. Tumor microenvironment in chemoresistance, metastasis and immunotherapy of pancreatic cancer. Am J Cancer Res. 2020;10(7):1937-1953.
- Hida K, Akiyama K, Ohga N, Maishi N, Hida Y. Tumour endothelial cells acquire drug resistance in a tumour microenvironment. J Biochem (Tokyo). 2013;153(3):243-249. doi:10.1093/jb/mvs152
- Guerrouahen BS, Maccalli C, Cugno C, Rutella S, Akporiaye ET. Reverting Immune Suppression to Enhance Cancer Immunotherapy. Front Oncol. 2020;9:1554. doi:10.3389/fonc.2019.01554
- Henke E, Nandigama R, Ergün S. Extracellular Matrix in the Tumor Microenvironment and Its Impact on Cancer Therapy. Front Mol Biosci. 2020;6:160. doi:10.3389/fmolb.2019.00160
- Wikman H, Vessella R, Pantel K. Cancer micrometastasis and tumour dormancy. APMIS. 2008;116(7-8):754-770. doi:10.1111/j.1600-0463.2008.01033.x
- Marin-Acevedo JA, Kimbrough EO, Lou Y. Next generation of immune checkpoint inhibitors and beyond. J Hematol OncolJ Hematol Oncol. 2021;14(1):45. doi:10.1186/s13045-021-01056-8
- Pàez-Ribes M, Allen E, Hudock J, et al. Antiangiogenic Therapy Elicits Malignant Progression of Tumors to Increased Local Invasion and Distant Metastasis. Cancer Cell. 2009;15(3):220-231. doi:10.1016/j.ccr.2009.01.027
- Ebos JML, Lee CR, Cruz-Munoz W, Bjarnason GA, Christensen JG, Kerbel RS. Accelerated Metastasis after Short-Term Treatment with a Potent Inhibitor of Tumor Angiogenesis. Cancer Cell. 2009;15(3):232-239. doi:10.1016/j.ccr.2009.01.021
- June CH, O’Connor RS, Kawalekar OU, Ghassemi S, Milone MC. CAR T cell immunotherapy for human cancer. Science. 2018;359(6382):1361-1365. doi:10.1126/science.aar6711
- Xu M, Zhang T, Xia R, Wei Y, Wei X. Targeting the tumor stroma for cancer therapy. Mol Cancer. 2022;21(1):208. doi:10.1186/s12943-022-01670-1
- Huang M, Shen A, Ding J, Geng M. Molecularly targeted cancer therapy: some lessons from the past decade. Trends Pharmacol Sci. 2014;35(1):41-50. doi:10.1016/j.tips.2013.11.004
- Huang M, Geng M yu, Ding J. Antitumor pharmacological research in the era of personalized medicine. Acta Pharmacol Sin. 2022;43(12):3015-3020. doi:10.1038/s41401-022-01023-0
- Zeng J, Hua S, Liu J, Mungur R, He Y, Feng J. Identification of core genes as potential biomarkers for predicting progression and prognosis in glioblastoma. Front Genet. 2022;13:928407. doi:10.3389/fgene.2022.928407
- Gatalica Z, Millis SZ, Vranic S, et al. Comprehensive tumor profiling identifies numerous biomarkers of drug response in cancers of unknown primary site: Analysis of 1806 cases. Oncotarget. 2014;5(23):12440-12447. doi:10.18632/oncotarget.2574
- Marx V. Method of the Year: spatially resolved transcriptomics. Nat Methods. 2021;18(1):9-14. doi:10.1038/s41592-020-01033-y
- Marx V. Researchers dig into cancer niches. Nat Methods. 2023;20(4):484-488. doi:10.1038/s41592-023-01834-x
- Hirz T, Mei S, Sarkar H, et al. Dissecting the immune suppressive human prostate tumor microenvironment via integrated single-cell and spatial transcriptomic analyses. Nat Commun. 2023;14(1):663. doi:10.1038/s41467-023-36325-2
- Biermann J, Melms JC, Amin AD, et al. Dissecting the treatment-naive ecosystem of human melanoma brain metastasis. Cell. 2022;185(14):2591-2608.e30. doi:10.1016/j.cell.2022.06.007
- Dobbin KK, Cesano A, Alvarez J, et al. Validation of biomarkers to predict response to immunotherapy in cancer: Volume II — clinical validation and regulatory considerations. J Immunother Cancer. 2016;4(1):77. doi:10.1186/s40425-016-0179-0
- Sankar K, Ye JC, Li Z, Zheng L, Song W, Hu-Lieskovan S. The role of biomarkers in personalized immunotherapy. Biomark Res. 2022;10(1):32. doi:10.1186/s40364-022-00378-0

