Standardized Preanalytical Coding (SPREC) in Tissue Biobanking
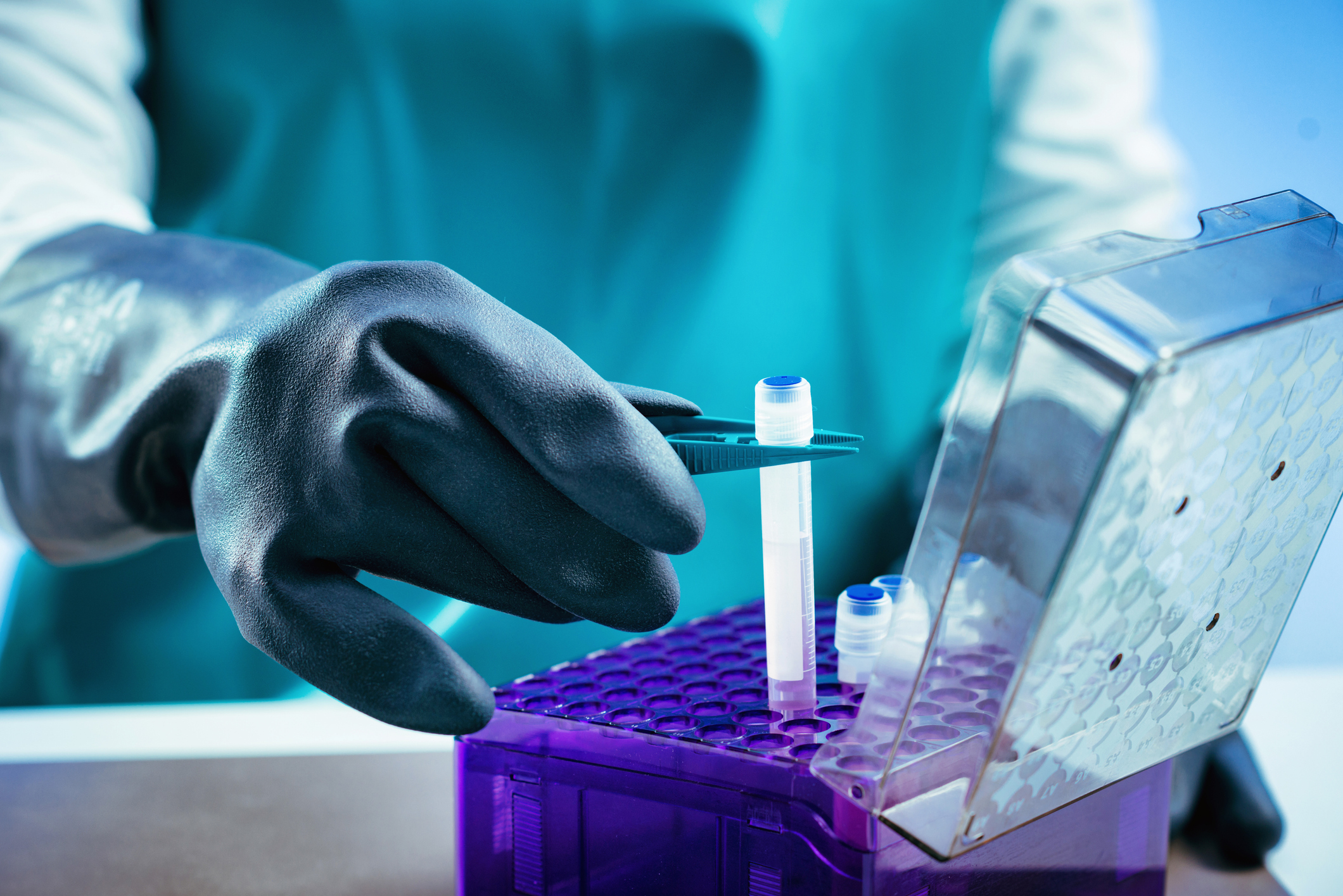
Tissue biobanking involves the collection, processing, storage, and study of biospecimens, such as human biofluids and solid tissue samples1. High biospecimen quality and collection of relevant patient data allow researchers and clinicians to tailor a personalized treatment for a given patient. Furthermore, biobanking allows researchers to assess differences by race and ethnicity for the patient cohorts, which helps deeply understand the heterogeneity within a disease subtype, expediting biomarker discovery and enhancing patient outcomes.
The Evolution of SPREC
The fidelity of biospecimen and the accuracy of stored data are paramount to allow researchers and clinicians to draw correct conclusions and apply patient-appropriate treatment. Variability in the pre-analytical processing and storage of biospecimen impacts data reproducibility 2, a perennial problem in biomedical research 3,4.
In 2009, Standardized Preanalytical Coding (SPREC) was developed by the International Society for Biological and Environmental Repositories (ISBER) Biospecimen Science Working Group to combat this problem and allow the potential of biobank research to be fully realized 5. SPREC guidelines have evolved to match technological advancements 6, but full international implementation is still lacking.
Here we highlight the importance of SPREC to tissue biobanking, researchers, and clinicians, and how it helps to promote the best possible patient outcomes through precision medicine.
Understanding Standardized Pre-analytical Coding
SPREC stands for Standardized Preanalytical Coding and its goal is to provide all relevant information regarding the procurement, storage, and processing of tissue samples prior to analysis. SPREC involves documentation of any variable that is likely to affect downstream results and is tailored to the sample type.
Non-SPREC-compliant laboratories can miss easily overlooked but crucial variability in pre-analysis processing. For example, researchers at the National Cancer Institute Biospecimen Preanalytical Variables Research Program within the NIH found that variability in the delay to fixation’ and ‘time in fixative’ of FFPE tissues adversely affected the quality of DNA and RNA, an essential parameter for downstream analysis 7.
How does SPREC work?
In the case of solid tissue samples, like tumor tissue samples, SPREC codes cover the following variables in this order:
- Type of sample: Example: Solid Tissue (Code: TIS)
- Type of collection: Example: Biopsy (Code: BPS)
- Warm Ischemia Time: Example: Not Applicable (e.g., biopsy) (Code: N)
- Cold Ischemia Time: Example: 2c–10c <60 min (Code: E4)
- Fixation/stabilization type: Example: Snap Freezing (Code: SNP)
- Fixation Time: Example: >72 h (Code: H)
- Long-term storage: Example: Paraffin Block (FFPE Tissues) (-35) to (-18)c: (Code: U)
Full Code: TIS-BPS-N-E4-SNP-H-U
A full set of tables providing sample codes for each parameter can be found in the 2018 publication, Standard PREanalytical Code Version 3.0.
Importance of Standardization in Tissue Biobanking
Practices in tissue acquisition, processing, and storage differ between institutions, and even within the same institutions (e.g., longer sample storage time during holidays). Different processing and record-keeping methods mean that samples cannot be accurately compared both within and across laboratories. Indeed, many samples are not even eligible for analysis due to a lack of pre-analysis documentation.
Data standardization using SPREC provides the following benefits:
- Improved data quality
- Improved sample comparability
- Improved research reproducibility
Data standardization of biobanking practices, particularly through SPREC, ensures that all relevant data is acquired and easily accessible. It allows scientists to understand which samples they can compare and which they can’t. This promotes good research conduct and enhances research reproducibility.
Furthermore, SPREC standardization confers a wide array of benefits to researchers, clinicians, and of course, patients.
Benefits of SPREC for Patients
High biospecimen quality in tissue biobanks leads to high-quality data. Improper labeling or poor storage of a patient tissue sample can lead to misdiagnosis and inappropriate treatment.
Indeed, a recent study found that around 795,000 deaths in US hospitals are attributable to misdiagnosis annually 8. Even if the type of sample is accurately assigned, if the storage is not compatible with the downstream analytical method the wrong conclusion can still be drawn. Thus, the need for accuracy and data standardization at every level is paramount. SPREC greatly diminishes the possibility of misdiagnosis by covering all bases and ensuring timely documentation, improving patient safety and outcome.
SPREC not only reduces the chance of error, it promotes the generation of high-quality research. The better the data, the more personalized and precise the medical intervention can be, and thus the best possible patient outcome can be achieved.
Why is Standardized Preanalytical Coding Vital for Researchers and Clinicians?
Tissue biobanking entails the storage of an increasingly large number of biospecimens and associated patient data. The need for data standardization and unified sample acquisition protocols is more pertinent than ever.
Adherence to SPREC means that researchers will know precisely where a sample comes from and how it was treated, facilitating good research conduct. Under SPREC, researchers studying a particular disease would have a global biospecimen pool to draw from, allowing them to select similarly treated samples for comparison.
In addition to providing confidence in sample quality, SPREC allows researchers to reliably study the effect of pre-analytical variables on sample quality 7. SPREC coding immediately indicates the laboratory maintains high standards and good research conduct.
Higher quality research ultimately leads to well-directed drug discovery programs giving clinicians more precise tools to treat their patients. SPREC also expedites biomarker discovery by giving researchers access to a larger set of comparable samples.
SPREC is essential to the continued improvement of our clinical arsenal and the pursuit of increasingly personalized treatment.
The Process of Implementing SPREC in Tissue Biobanking
SPREC is implemented during the processing and labeling phase of tissue biobanking and can easily be applied alongside existing in-house barcoding methodology to add another layer of data quality. Where preexisting data is stored, it can be retrofitted to conform to SPREC, with unknown parameters designated with the code “X”. To be fully SPREC compliant however, laboratories must record all parameters outlined in the Standard PREanalytical Code Version 3.0.

International standards organizations play a central role in SPREC adoption. Ultimately it is these organizations that will usher in a universal infrastructure for tissue biobanking. SPREC has already been successfully implemented into the “Minimum data set for sharing biobank samples, information, and data” (MIABIS) and implemented as the national standard in Sweden in addition to many biobanks in the US, Korea, Europe, and Australia 9,10.
Collaboration and Data Sharing
SPREC implementation means that biobanks, research institutions, and healthcare providers can collaborate effectively. A standardized system removes the need to decipher in-house codes and rely on incomplete documentation. With SPREC researchers have access to large, reliable, and diverse datasets for research.
A greater sample size means greater statistical power and thus more reliable conclusions. Data derived from low-quality, untraceable samples give you nothing. As any bioinformatician worth their salt will tell you: “Garbage in – Garbage out.”
The Future Trends and Innovations
Biobanking is a far from optimized process, though with the implementation of data standardizations like SPREC the future is bright despite the challenges. With the advent of increasingly powerful computers and AI, analysis of huge sets of biobank-derived data for hypothesis generation are on the horizon 11. These biobanking trends highlight the urgent need for international data standardization and the evolution of our practices. Indeed SPREC is already in its third iteration and we can expect further advancements in SPREC as our technological capabilities improve 6.
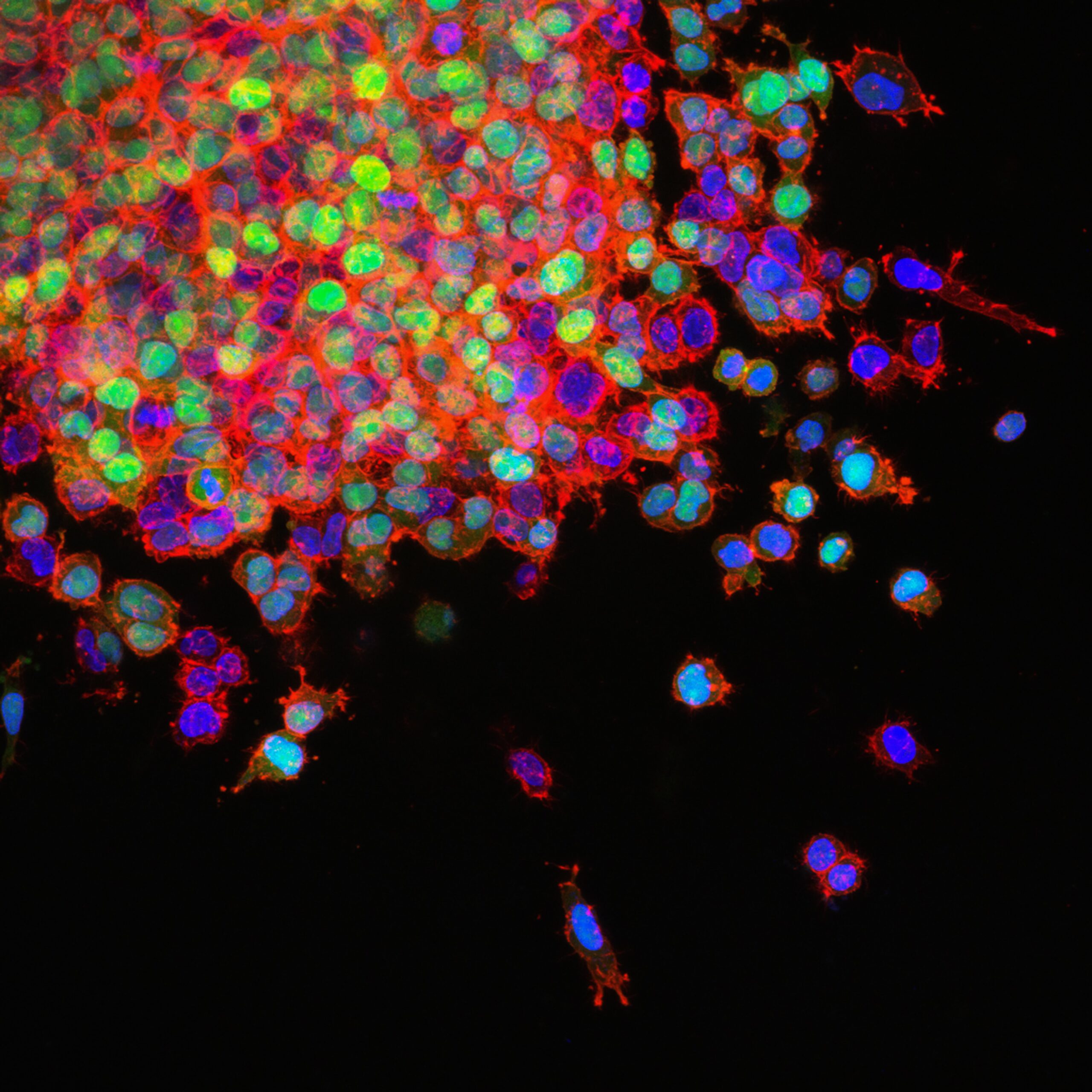
Technological advancements mean that an increasingly large array of samples can be acquired. For example, circulating tumor cells, i.e., cancer cells that have broken away from the primary tumor and entered circulation, are an area of emerging interest. Metastasis is the leading cause of cancer-associated mortality and establishing a biobank of circulating tumor cells (i.e., during the metastatic process) would lead to a greater understanding of how cells gain metastatic potential 12.
Conclusion
SPREC is an essential tool for standardizing tissue biobanks, ensuring all relevant variables are recorded in an accurate and timely manner. SPREC means that researchers have access to a greater number of reliable samples which in turn allows them to draw reliable conclusions from their analyses. The result will be a wider variety of personalized treatments for clinicians to call upon, with ever-improving patient outcomes.
To learn more about how quality human biosamples can enhance the quality of your research, visit our dedicated product page and request a quote, or get in touch today.
References
- Skoworonska, M. et al. Real-life data from standardized preanalytical coding (SPREC) in tissue biobanking and its dual use for sample characterization and process optimization. J. Pathol. Clin. Res. 9, 137–148 (2023).
- Moore, H. M. et al. 2009 Biospecimen research network symposium: advancing cancer research through biospecimen science. Cancer Res. 69, 6770–6772 (2009).
- Prinz, F., Schlange, T. & Asadullah, K. Believe it or not: how much can we rely on published data on potential drug targets? Nat. Rev. Drug Discov. 10, 712 (2011).
- Betsou, F. et al. Standard Preanalytical Coding for Biospecimens: Defining the Sample PREanalytical Code. Cancer Epidemiol. Biomarkers Prev. 19, 1004–1011 (2010).
- Betsou, F. et al. Standard PREanalytical Code Version 3.0. Biopreservation Biobanking 16, 9–12 (2018).
- Carithers, L. J. et al. The Biospecimen Preanalytical Variables Program: A Multiassay Comparison of Effects of Delay to Fixation and Fixation Duration on Nucleic Acid Quality. Arch. Pathol. Lab. Med. 143, 1106–1118 (2019).
- Newman-Toker, D. E. et al. Burden of serious harms from diagnostic error in the USA. BMJ Qual. Saf. bmjqs-2021-014130 (2023) doi:10.1136/bmjqs-2021-014130.
- Norlin, L. et al. A Minimum Data Set for Sharing Biobank Samples, Information, and Data: MIABIS. Biopreservation Biobanking 10, 343–348 (2012).
- Lehmann, S. et al. Standard preanalytical coding for biospecimens: review and implementation of the Sample PREanalytical Code (SPREC). Biopreservation Biobanking 10, 366–374 (2012).
- Eisenstein, M. Machine learning powers biobank-driven drug discovery. Nat. Biotechnol. 40, 1303–1305 (2022).
- Deng, Z., Wu, S., Wang, Y. & Shi, D. Circulating tumor cell isolation for cancer diagnosis and prognosis. EBioMedicine 83, 104237 (2022).
- Annaratone, L. et al. Basic principles of biobanking: from biological samples to precision medicine for patients. Virchows Arch. Int. J. Pathol. 479, 233–246 (2021).

