How Biospecimens Support Biomarkers Development?
One of the main applications of human-derived biosamples in biomedical research is in the discovery and validation of new biomarkers. This is especially true for the oncology field, where biospecimens support biomarkers development from the discovery stage through validation, and ultimately during implementation into diagnostics and choice of targeted therapy by providing scientists and clinicians with a glance into each individual's unique genetic and molecular background.
When we speak about the role of biospecimens in the advancement of personalized precision medicine, we can’t avoid the topic of biomarkers. The term biomarker indicates a molecular signature (DNA, RNA, protein, lipid, metabolite) that can be objectively measured. Its levels are an indication of a normal physiological process, an abnormal pathological condition, or a response to a therapeutic intervention.
Biomarkers have become an indispensable part of today’s research and care process. Because of cancer’s significant heterogeneity, biomarker characterization is essential for adequate patient stratification and treatment choice.
The use of some cancer biomarkers is a well-established practice, but the latest advances in high-throughput sequencing and multi-omic analysis are driving biomarker discovery and validation to new frontiers. Here, we look at the classification of biomarkers and the current trends and obstacles in their discovery and validation process.
How do biospecimens support biomarkers development?
Biospecimens, biomarkers and precision medicine are tightly interconnected and codependent and are the driving force of modern and future healthcare.
It was the rise of Next Generation Sequencing (NGS) and other high-throughput screening methods such as metabolomics and proteomics that kicked off the expansion of the biomarkers field. The successful identification of unique molecular signatures initiated the establishment of personalized and targeted therapies. The identification of biomarkers is only possible if scientists can screen large cohorts of healthy and diseased patients to identify these molecular footprints.
The obvious benefits of these novel therapeutic approaches for both patients and healthcare systems iс on its end driving the need for more and better biomarker identification, as well as understanding and targeting the molecular mechanisms causing a disease rather than just treating the symptoms. Thus an interlinked circle is formed centered around the patient’s unique molecular profile.
Applications and types of cancer biomarkers
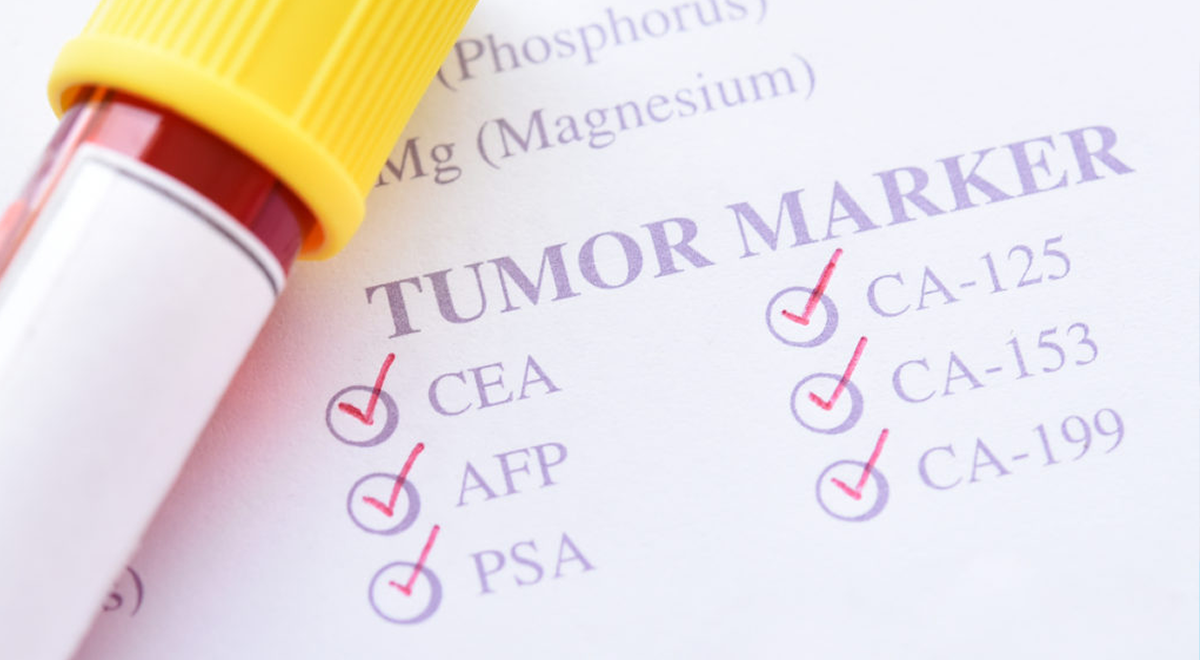
Biomarkers are classified depending on their use, and often one biomarker can have multiple applications.
Risk biomarkers, for example, are informative for quantifying potential risks of developing a particular disease. A well-established example in clinical practice is detecting mutations in the BRCA1/2 gene associated with an increased risk of breast/ovarian cancer development.
If used to confirm a diagnosis, cancer biomarkers are also diagnostic. PSA (Prostate-Specific Antigen) and CA-125 (Cancer Antigen 125) are used for prostate and ovarian cancer diagnostics. Both biomarkers also have monitor applications, as they are used to follow-up with patient responses and cancer recurrence during or after treatment.
Biomarkers can be prognostic if used to inform clinicians on outcomes such as survival expectancy and recurrence. Predictive biomarkers are used to predict the potential responsiveness to a specific therapy. The human epidermal growth factor receptor 2 (HER2) is used for the selection of an effective HER2 targeting treatment in breast cancers overexpressing this marker. HER2 is also an indication of a more aggressive type of breast cancer 1, 2 .
Biomarkers discovery and validation process
Discovery phase is the initial step in a biomarker's journey to clinics. It includes the preclinical discovery research during which a biomarker candidate or a panel of candidates are identified.
Afterward, these candidate biomarkers undergo analytical and clinical validation processes inorder to make it into the FDA's list of qualified biomarkers. The first one evaluates how accurately and reliably the biomarker candidate can be measured by a clinical testing platform. This analysis often compares results obtained from measuring the biomarker with the technique used in the discovery phase and with the clinical platform to determine the reproducibility of the results.
The clinical validation entails assessing how robust and correlated to the clinical phenotype the test results are. Once a biomarker is validated on both parameters, it is ready to be implemented in clinical care 3, 4 .
Critical problems in biomarkers discovery and validation
The constantly improving high-throughput methods and large cohort screening studies that are being performed over the last few years have generated an immense amount of data and possibilities for new biomarker discovery. Despite being a key tool for clinical progress, this process often gives disappointing results mainly due to the disproportion in the number of biomarkers identified in the early discovery phase and the ones that make it to clinical use.
It is an established consensus among the biomarkers science community that a major issue is poor study design, especially during the early discovery phase. Often time and cost restrictions drive the use of samples previously collected for other purposes. This repurposing of biomaterials creates significant bias due to differences in the way samples are being collected, stored, and processed. Such practices ultimately cause non-reproducible results during validation steps and failure to reach clinical implementation.
Overcoming these issues requires increased attention to detail during the study design. The purpose of the biomarker should be well-defined from the start, and the study designed accordingly. Well-defined inclusion/exclusion criteria and sample size for the biospecimen collection are crucial as well as attention to internal validation during the discovery phase 5-7.

How can we assist your biomarker discovery?
At Audubon Bioscience, we understand the importance of biomarkers in clinical practice and biomedical progress. We are determined to assist in the conduct of efficient discovery studies by providing comprehensive biospecimen collections designed specifically for your needs. For more information consult our collection capacities or get in touch with our team!
References:
- Liu, D. Cancer biomarkers for targeted therapy. Biomark. Res. 7, 1–7 (2019).
- Ricciuti, B., Leonardi, G. C. & Brambilla, M. Emerging Biomarkers in the Era of Personalized Cancer Medicine. Dis. Markers 2019, 5907238 (2019).
- Goossens, N., Nakagawa, S., Sun, X. & Hoshida, Y. Cancer biomarker discovery and validation. Transl. Cancer Res. 4, 256–269 (2015).
- Hayes, D. F. ScienceDirect Biomarker validation and testing. Mol. Oncol. 9, 950–6 (2015).
- Schully, S. D. et al. Leveraging biospecimen resources for discovery or validation of markers for early cancer detection. J. Natl. Cancer Inst. 107, 1–7 (2015).
- Pepe, M. S., Feng, Z., Janes, H., Bossuyt, P. M. & Potter, J. D. Pivotal evaluation of the accuracy of a biomarker used for classification or prediction: Standards for study design. J. Natl. Cancer Inst. 100, 1432–1438 (2008).
- Pepe, M. S., Li, C. I. & Feng, Z. Improving the quality of biomarker discovery research: The right samples and enough of them. Cancer Epidemiol. Biomarkers Prev. 24, 944–950 (2015).

