Blood Cancers Overview – History, Advancements and Challenges
Every September, the world marks Blood Cancer Awareness Month. This year, Audubon Bioscience joined the initiative and its efforts to inform patients about this variable group of malignant pathologies.
We support the campaign with this article, which briefly overviews the different types of blood cancers, the most common risk factors, and symptoms, allowing for early detection and better chances of successful treatment. Moreover, we take a look at the treatment history of blood cancers as well as the latest advances and persisting challenges.
Nature and classification of blood cancers
Blood cancers are a large group of pathologies affecting the blood cells and causing the uncontrolled division of a particular subset of hematological cells and thus affecting their regular activity. Blood malignancies start in the bone marrow, where blood cells are produced and later affect the entire body.
Depending on the type of blood cell they affect, blood malignancies are divided into three main types - Leukemias, Lymphomas, and Myelomas 1.
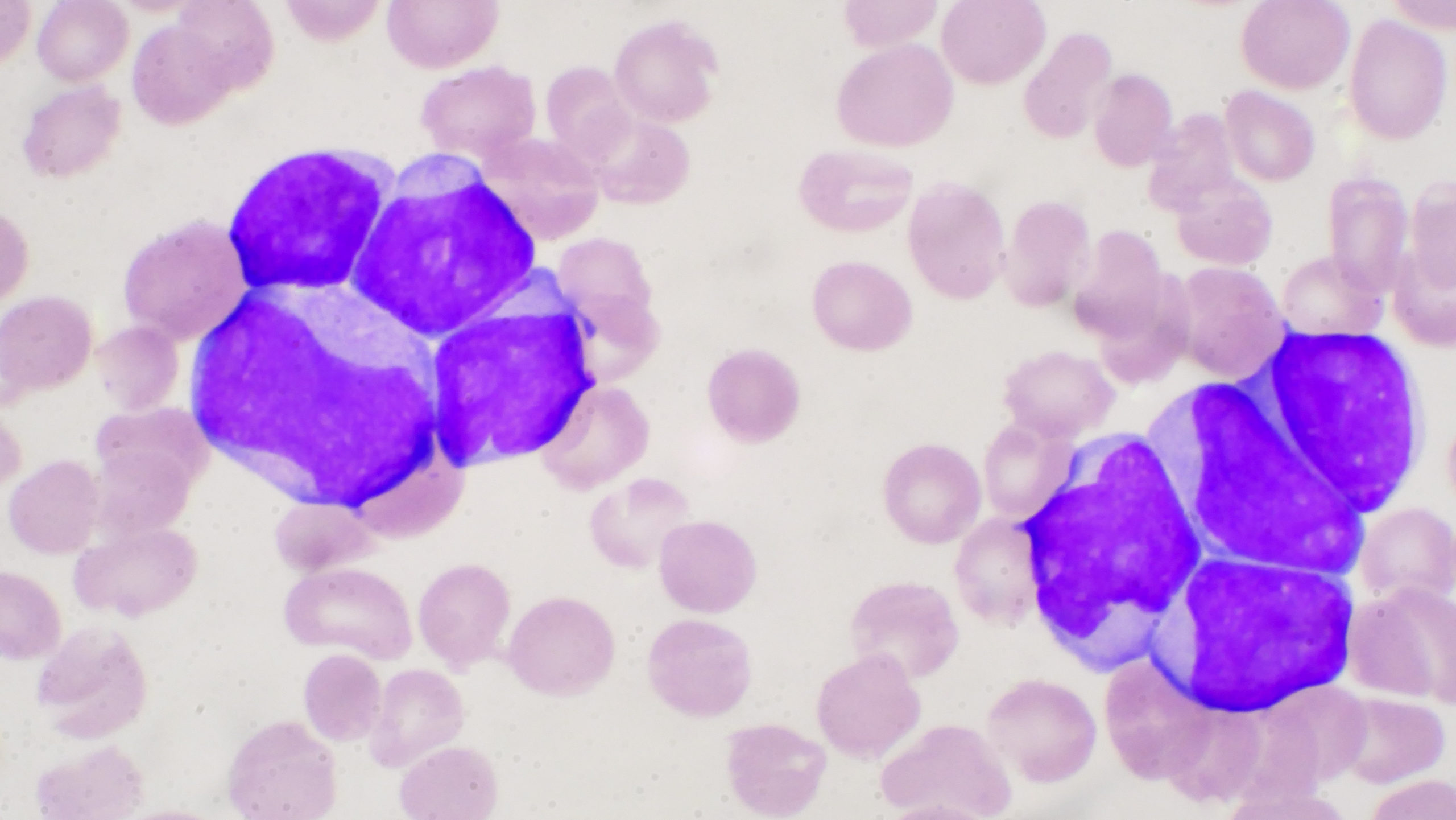
Leukemias are caused by abnormal expansion of cancerous white blood cells or leukocytes that are not functioning properly. Subsequently, leukemias are divided into many sub-groups. The first level of differentiation is between acute and chronic, including Acute myeloid leukemia (AML), Acute lymphocytic leukemia (ALL), Chronic lymphocytic leukemia (CLL), Chronic myeloid leukemia (CML), but can also be divided in function of the affected cell type as, for example, Prolymphocytic leukemia (PLL), Large granular lymphocytic (LGL), Hairy cell leukemia (HCL), and Myelodysplastic syndromes (MDS). Some leukemias affect only adults, while others, such as ALL and AML, also affect children and are the most common type of cancer among children and teenagers.
Lymphomas affect the immune systems by causing the uncontrolled production of abnormal lymphocytes. The cancerous lymphocytes travel through the blood and the lymphatic system to various body parts, where they accumulate into cancerous formations.
The British doctor Thomas Hodgkin first described this disease in 1832. More than 100 types of lymphomas have been identified since then. However, the two main classes are Hodgkin and Non-Hodgkin lymphoma (NHL). The main difference between these two forms is the presence of Reed-Sternberg cells in Hodgkin patients and their absence in NHL ones. Reed-Sternberg cells are large abnormal lymphocytes containing more than one nucleus.
Among the Hodgkin lymphoma cases, classical Hodgkin lymphoma is the predominant form accounting for more than 90% of all cases. Still, several other forms of Hodgkin lymphoma exist as well: nodular sclerosis Hodgkin lymphoma, mixed cellularity Hodgkin lymphoma, lymphocyte-rich Hodgkin’s disease, and lymphocyte-depleted Hodgkin’s disease.
NHL is the more common form of lymphoma and is divided into B-cell and T-cell lymphoma. B-cell NHL accounts for more than 80% of NHL cases in the U.S. and can be further subdivided into a plethora of subtypes, including diffuse large B-cell lymphoma (DLBCL), primary mediastinal B-cell lymphoma, follicular lymphoma, small lymphocytic lymphoma, and chronic lymphocytic leukemia, marginal zone lymphoma, mantle cell lymphoma, Waldenström’s macroglobulinemia, and Burkitt lymphoma. Although sparse, several types of T-cell NHL lymphomas exist, such as peripheral T-cell lymphoma, anaplastic large cell lymphoma, angioimmunoblastic lymphoma, and cutaneous T-cell lymphoma. NHL is usually diagnosed in patients over 60, whereas the Hodgkin form can affect younger patients.
Multiple myeloma (MM), also known as myeloma, is characterized by the uncontrolled division of the antibody-producing plasma cells within the bone marrow. MM can be divided into two classes: Hyperdiploid (HMM) and Non-hyperdiploid or hypodiploid. In the case of HMM, the cancerous myeloma cells have more chromosomes than normal. It is usually the less aggressive MM type. Non-hyperdiploid myeloma cells have fewer chromosomes, and this is the more aggressive form of the disease. The two conditions have relatively similar incidences of approximately 40%. Myelomas can additionally be categorized in more subtle groups such as Light Chain Myeloma, where patients can only synthesize immunoglobulins light chains, Non-secretory Myeloma, Solitary Plasmacytoma, Extramedullary Plasmacytoma, and the sporadic forms of Immunoglobulin D (IgD) Myeloma and Immunoglobulin E (IgE) Myeloma. Several precancerous conditions are associated with MM, such as Monoclonal Gammopathy of Undetermined Significance (MGUS) and Smoldering Multiple Myeloma (SMM).
The long list of conditions defined as blood cancers clearly shows the need for correct diagnosis and an effective precision treatment assignment.
History of blood cancer therapies
Chemotherapy, radiotherapy, and bone marrow transplants are the classical methods for treating blood cancers. The first radiation therapies for lymphomas date back from the 20th century. Chemotherapy roots can be traced back to World War I, when it was discovered that the deadly mustard gas blocks hematopoiesis. This observation led to the idea that small amounts of the weapon could be used against blood cancers. And so, nitrogen mustard treatment became the first successful chemotherapy for lymphoma 2.
Bone marrow transplants began in the 1960s. Their discovery is also connected to another humanitarian disaster -- World War II, when healthy donor transplants successfully replaced the destroyed bone marrow of atomic bomb survivors 3.
Notably, blood cancer therapies opened the gates for targeted and precision treatments of malignant conditions. In 2001, the FDA approved the very first targeted therapy - Imatinib or Gleevec against NHL. The drug is a first-generation tyrosine kinase inhibitor and specifically targets BCR-ABL tyrosine kinase. Due to its impressive success rates, Gleevec has transformed the field of NHL treatment and today is also approved for the treatment of gastrointestinal cancers 4, 5.
The next blood cancer treatment breakthrough was in 2002, when Rituximab, a monoclonal antibody targeting CD-20 positive B-cells, was approved as a companion treatment of chemotherapy in older DLBCL patients 6. The improved survival rates in this patient group were confirmed in patients of all ages, and Rituximab/chemotherapy became a standard treatment for this lymphoma type. In the same year, the approval of Zevalin marked another success for lymphoma treatment. Zevalin is a monoclonal antibody against CD-20 coupled to radioactive material and thus selectively killing only CD-20 positive B-cells 4.
Blood cancers play a historical role in the development of targeted therapies. Notably, such therapies were first approved for blood malignancies before the finalization of the Human Genome Project in 2003, an event considered to be the cornerstone for personalized medicine and targeted therapies.
Current advances and persistent challenges
Thanks to the success of the Human Genome Project and the advancements made in cancer immunotherapy, today, the list of targeted and innovative therapies against blood cancer has grown immensly, including Chimeric Antigen Receptor T-cells (CAR T-cell) treatments, oral therapies by targeted agents, checkpoint inhibitors and more monoclonal antibodies 7, 8.
In 2021 several targeted therapies against blood cancers were approved. In January, the monoclonal antibody, daratumumab (Darzalex), in combination with other drugs was approved for a subset of adult multiple myeloma patients. In March, the CAR T-cell therapy, idecabtagene vicleucel (Abecma), and monoclonal antibody, isatuximab (Sarclisa), were licensed to treat the same blood cancer class. And since this year, large B-cell lymphoma can be treated with the antibody-drug conjugate, loncastuximab (Zynlonta), and the CAR T-cell immunotherapy, lisocabtagene maraleucel (Breyanzi).
The success of such therapies has dramatically improved the lives of blood cancer patients, and survival rates have impressively increased over the past 20 years. Despite these successes, current statistics show that in the U.S., every 3 minutes, someone is diagnosed with blood cancer, and more than ⅓ of blood cancer patients don’t survive longer than five years after they are being diagnosed.
A major challenge for blood cancer prevention is the lack of early detection testing, which further stresses the need for knowing the risk factors and early symptoms and reporting them to your doctor.
For example, high levels of radiation are correlated to the development of AML and ALL. Genetic syndromes such as Down syndrome are also associated with an increased risk of developing ALL. In lymphoma, radiation and some chemicals are described to be involved in the disease development. A weakened immune system is also linked with the development of both Hodgkin and Non-Hodgkin forms of lymphoma.
When it comes to symptoms, they are quite variable 9 and depend on the type of blood cancer. Main common signs for all blood-related malignancies include:
- Unexplained fever or chills
- Persistent fatigue, weakness
- Anemia
- Frequent infections
- Excessive sweating, especially at night
- Bruising or bleeding easily
- Unexplained weight loss
- Loss of appetite
- Swollen lymph nodes and swollen abdomen
Some symptoms are more specific and associated with a particular class of hematological cancer. For example, tiny red spots in the skin (petechiae) are distinctive for leukemias. In contrast, patients with lymphoma experience unexplained cough and breathing problems, and swollen lymph nodes are mainly found around the neck and armpits. Multiple myeloma is associated with excessive thirst, bone pain, especially in the spine or the chest, and leg numbness.
The large variability of blood cancers, the associated risk factors and multiple early symptoms make them hard to detect. Therefore, it is essential for individuals to do regular blood count checkups, know the early warning signs, and consult a medical professional if you experience any of them.
Audubon Bioscience supports Blood Cancer Awareness Month

Audubon Bioscience supports blood cancer research daily with our blood and bone marrow custom collection and processing services. Our mission and actions are strongly oriented towards supporting the patient's well-being. Because of this, we join all awareness campaigns aiming to help understand serious health issues and bring better solutions to patients.
For more resources on how blood samples contribute to discovering life-saving therapies, visit our blog page. In addition, you can learn more about the roles of doctors and patients in supporting biomedical research at our dedicated pages.
For any other questions you might have, please get in touch with us. We will be happy to help you!
References:
- “September Is Blood Cancer Awareness Month | Leukemia and Lymphoma Society.” Leukemia and Lymphoma Society, 2021, www.lls.org/article/september-blood-cancer-awareness-month.
- “History of Cancer Treatments: Chemotherapy.” American Cancer Society, 2014, www.cancer.org/cancer/cancer-basics/history-of-cancer/cancer-treatment-chemo.html
- Henig, Israel, and Tsila Zuckerman. “Hematopoietic Stem Cell Transplantation—50 Years of Evolution and Future Perspectives.” Rambam Maimonides Medical Journal, vol. 5, no. 4, 2014, p. e0028. Crossref, doi:10.5041/rmmj.10162.
- “Cancer Progress Timeline.” American Society of Clinical Oncology, 2020, www.asco.org/research-guidelines/cancer-progress-timeline/targeted-drugs.
- “Gleevec: The Breakthrough in Cancer Treatment.” Nature, 2008, www.nature.com/scitable/topicpage/gleevec-the-breakthrough-in-cancer-treatment-565.
- Smith, Mitchell R. “Rituximab (Monoclonal Anti-CD20 Antibody): Mechanisms of Action and Resistance.” Oncogene, vol. 22, no. 47, 2003, pp. 7359–68. Crossref, doi:10.1038/sj.onc.1206939.
- Cancer Treatment Centers of America (CTCA) Comprehensive Cancer Care Network. “What You Need to Know about Breakthroughs in Blood Cancer Treatments.” Cancer Treatment Centers of America, 28 June 2016, www.cancercenter.com/community/blog/2016/06/what-you-need-to-know-about-breakthroughs-in-blood-cancer-treatments.
- Pancholi, Neha J., PhD. “AACR Meetings Feature Latest Advances in Blood Cancer Research.” American Association for Cancer Research (AACR), 12 May 2021, www.aacr.org/blog/2021/05/07/aacr-meetings-feature-latest-advances-in-blood-cancer-research.
- “Blood Cancers: Symptoms, Diagnosis and Treatment.” Yale Medicine, 28 Oct. 2019, www.yalemedicine.org/conditions/blood-cancers.

